RED LEG (Conditions, Irritations & Infections)

Welcome to the turning of summer into fall! As we are encountering everything from colorful trees to colorful politicians, let’s turn our attention to the colorful legs that can sometimes be quite perplexing. Just as a red wound bed can represent different situations, so can redleg skin. In this blog post, we will concentrate on the red leg, trying to distinguish between conditions, irritations, and infections.
Hemosiderin

Venous Dermatitis

This can also be confused with cellulitis due to its red, swollen, irritated skin.
Lipodermatosclerosis

There is both an acute and chronic phase. The acute phase presents with redness, pain and inflammation, while the chronic phase is characterized by fibrotic, indurated skin that is very difficult to mobilize. The acute phase can be confused with cellulitis due to similar presentation. Usually a good history can differentiate between the two.
Lymphedema

See the National Lymphedema Network for a complete discussion of this difficult condition.
Cellulitis

The Cleveland Clinic gives a good synopsis of key points:
- Cellulitis is rarely bilateral
- Patients with cellulitis often have systemic symptoms, such as fever and leukocytosis.
- A chronic course points to a diagnosis other than cellulitis
- Plaques with a “bound-down” appearance or dark pigmentation point to a chronic disease rather than acute
- Stasis dermatitis is the most common mimic of cellulitis
CCJM 2012 Aug;79(8):547-552
The picture on the left shows a woman that has a hot, painful leg that is significantly different than her other leg (which has definite hemosiderin changes of its own). The erythema is not confined to any hemosiderin discoloration, but involves the entire lower leg and foot. She needed antibiotics immediately to treat her infection.
Dependent Rubor

In those with a dark complexion, it is important to compare skin color to healthier areas. Sometimes the rubor can be mistaken for erythema that would more indicate infection. This patient has some significant ischemia in her first toe. Undoubtedly the ischemic limb will be cool to touch vs. the infected limb that would be warm or hot to palpation.
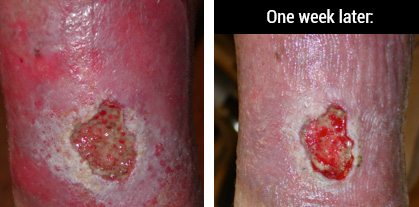
It is not always easy to differentiate a red leg with cellulitis from a red leg with hemosiderin staining, lipodermatosclerosis, venous dermatitis, or any number of skin conditions that share some of the same characteristics. Consider the treatment history and the response (or lack thereof) to antibiotics. If onset is slow and response is negligible to treatment, then consider a non-cellulitis diagnosis. Consult with dermatology and vascular to rule out various conditions.
I hope this helps you to begin to recognize and differentiate between the conditions with red legs.
This blog post was written by Robin Carlson, PT CWS
What is PT CWS? Physical Therapist and Certified Wound Specialist
Shareable Infographic



