Oh the Holidays…Oh the Chronic Wound Pain!
The holiday season is a time of joy and love, but for people with chronic pain during the holidays it can be a time of stress, depression, frustration, and increased pain. Pain in chronic wounds such as arterial insufficiency ulcers, venous leg ulcers, and diabetic foot ulcers can reduce their quality of life. The pain in these types of chronic wounds causes inflammation and damage to the body tissue or peripheral nerve disease, all of which can have a negative impact on wound healing. The individual can also experience difficulty with concentration, poor sleeping pattern (1) and affect the healing process. (2). Pain can also be exacerbated by some dressing changes as well as the periwound skin, area around the wound.
Prompt treatment is key to pain management. Further management should focus on appropriate dressing as well as pain medication. The goal is to provide maximum relief with minimum side-effects. (3)
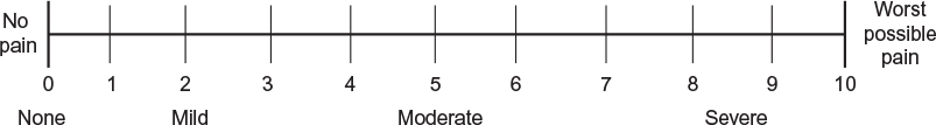
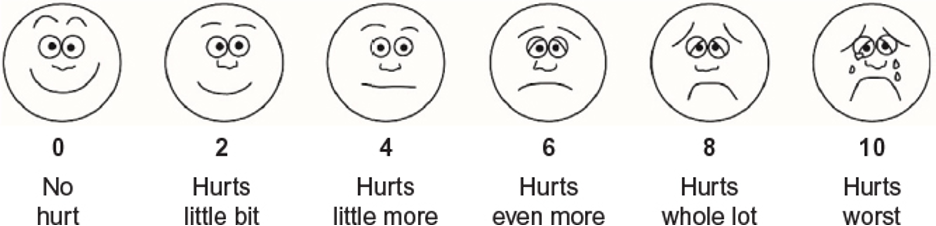
Over the last few years there is an increased awareness of pain assessment and management in enhancing the quality of life and improving wound healing outcomes. A number of tools are available, below are two most widely used assessments.
Numeric Pain Rating Scale.
Wong-Baker FACES® Pain Rating Scale. (4)
So, what can you do to decrease the stress, depression, frustration, and increased pain while you prepare for the holidays and enjoy them as well?
If you’re planning a shopping spree consider non-steroidal anti-inflammatory drugs such as acetaminophen (Tylenol)/ ibuprofen (motrin/advil) (5) at least a half hour before you venture out, this gives the drug a chance to work. Take a break during the shopping spree, relax and stretch out your legs.
Preparing your favorite dishes for the holidays, you’re going to be on your feet for quite a while, consider applying compression stockings over your wound dressing. The compression reduces swelling in the feet and ankles
Minimizing pain during dressing changes. Avoid dressings that can stick to the wound, such as gauze or dressings with adhesive borders. Dressings such as silicone, collagens, alginates or hydrofibers will be less traumatic. Also consider the frequency of dressing changes, how often is the dressing changed. The goal is to select dressings that minimize trauma during dressing change and protect the periwound skin.
This blog post was written by Mary Forman, BSN, MBA, WOC, CWCN – EO2 Clinical Specialist
What do her credentials mean? WOC is a wound, ostomy, continent nurse. CWCN is a certified wound care nurse. Mary has been working in wound care for 30 years.
References:
- Mason V (2009) Psychological factors of pain perception, communication and responses to treatment. In: White R, Harding K (eds) Trauma and Pain in Wound Care Vol 2. Aberdeen: Wounds UK
- Eagle M (2009) Wound assessment: the patient and the wound. Wound Essentials; 4: 14-18.
- Serena, T., YaakovR. Aslam, S., Aslam, R. Preventing, minimizing, and managing pain in patients with chronic wounds: challenges and solutions. 25 July 2016 Volume 2016:3 Pages 85—90
- WongBaker FACES Foundation (2015). WongBaker FACES® Pain Rating Scale. Available from: http://www.WongBakerFACES.org
- World Health Organization [https://www.who.int/]. WHO’s Pain Ladder. Last Update: May 18, 2021